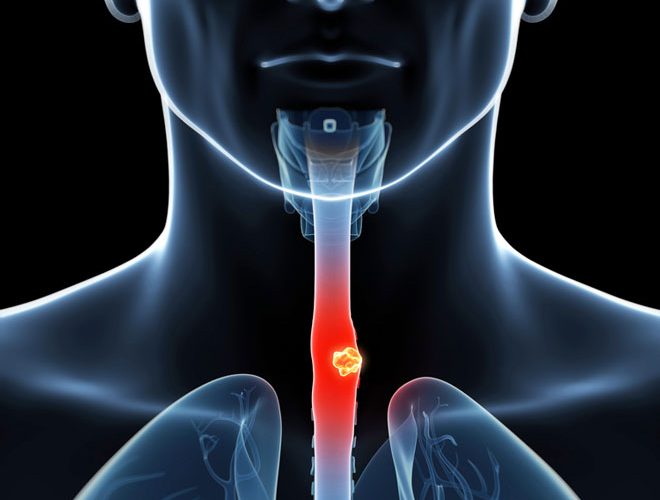
If someone feels food getting stuck in the chest or upper abdomen while eating this may be due to an oesophageal cancer. Most of these people would have a long standing history of reflux prior to this or might have accidentally or intentionally taken some corrosive substance previously. However some might not have such history as well. Some may be having a family history of cancers especially oesophageal cancers. Smoking, certain food habits – Far Asians; Japanese, who consume lot of smoked food are more vulnerable to get oesophageal cancer.
The feeling of food getting stuck while eating normally start with solid food and gradually progress to liquids as well. They may progress to develop regurgitation or vomiting of undigested food immediately after eating. These patients may loose weight mainly not because of loss of appetite but due to avoidance of food due to discomfort or fear of vomiting. Patient may feel hungry all the time.
If any of the above symptoms are present you should see your doctor immediately. Your family doctor will take a careful history and do an examination of you. Doctor will look for a mass in your neck or for any other lump anywhere else. If he feels it necessary you will get referred to a specialist doctor to carry out a camera test on you. This will help in diagnosing whether one is having cancer or not. If a cancer is diagnosed at its precancerous stage or at early stages this can be successfully treated.
At the endoscopy a biopsy will be done from the growth to find the tissue type by looking at it under the microscope (Histology). A CT scan will be done to assess the extent of the spread and the stage of the disease. Depending on the tissue type and stage of the cancer it will be decided by a group of specialists (Multi Disciplinary Team – MDT) how to treat the patient. This can be either a surgery straight away or after chemotherapy. Another type of cancer may need radiotherapy. If patient is not fit for a major operation; they will decide to do a ‘bridging’ procedure of feeding the patient by placing a special device across the cancer to overcome the block called a ‘stent’ and optimize him for surgery. Sometimes this may be done through a tube (Naso-Gastric tube – NG tube) passed through your nose to stomach or a tube inserted into the stomach (Feeding gastro stormy or a PEG- Percutaneous Endoscopic Gastrostomy) or to small bowel (Feeding jejunostomy) through the abdominal wall.
Sometimes it may not be possible to operate and remove the cancer if it is too advanced and spread to surrounding structures and to other organs of the body. These instances it will be decided to give only chemotherapy or radiotherapy and make the patient comfortable with other supportive therapy at the MDT – ‘Palliative care’.